Procedures
As a cervical spine specialist, Dr. Wright has performed more than 2,500 cervical spine surgeries. He is considered one of the leading experts in the field and has special expertise in a number of procedures, including the following:
ANTERIOR CERVICAL DISCECTOMY AND ARTHROPLASTY
Anterior cervical discectomy and arthroplasty is typically recommended for patients who have disc herniation, neck injury, or degenerative disc disease causing chronic pain that hasn’t been relieved through non-surgical treatments.
Dr. Wright performs the procedure as an alternative to fusion surgery because it provides patients numerous benefits, including:
-
-
-
- Preserved motion
- Fewer of the complications or issues sometimes associated with a bone graft or fusion
- Reduced strain on adjacent tasks
-
-
The procedure is designed to relieve the pressure on your spinal cord or nerves that are causing the pain, numbness, and weakness that can radiate to your shoulder, arm, and hand.
Procedure
During the procedure, Dr. Wright removes the damaged disc and replaces it with an artificial one, which is designed to replicate the natural motion of the spine. After he removes the damaged disc, he will smooth away any bone spurs and then place and anchor the artificial disc in the empty space that is left. Dr. Wright then closes the incision and covers it with a dressing.
Recovery
Since disc arthroplasty does not reduce motion in the neck, there is a lower risk of developing wear and tear at the other levels of your neck (adjacent segment disease) in the future. But disc arthroplasty is not for every patient; Dr. Wright will discuss with patients why they are, or are not, candidates for cervical disc replacement.
Research
As an expert on this procedure, Dr. Wright has been part of several FDA trials, and has presented the research at the following national meetings:
-
-
- Wright, N.M., W.S. Edwards, C.S. Theofilos, R. Garcia, and L.L. Thibodeau. Two year results from five IDE sites: CerviCore intervertebral disc vs. fusion. 2010 AANS/CNS Spine Section annual meeting, 2/10.
- Garcia, R., Wright, N.M., Gratch, M., and Fishgrund, J.. Cervicore Disc Replacement vs. Fusion: One-Year Outcomes from Four US IDE Study Sites. 2009 CSRS annual meeting, 12/09.
- Wright, N.M., Abitbol, J.J., Baldwin, N.G., and Youssef, J.A.. CerviCore disc replacement vs. fusion for single-level cervical radiculopathy: one-year outcomes from four study sites in a prospective randomized controlled trial. 2009 AANS/CNS Spine Section annual meeting, 3/09.
- Wright, N.M., Garcia, R., Gratch, M.J., and Fischgrund, J.S.. CerviCore disc replacement vs fusion for cervical nerve root compression: clinical and radiographic outcomes from a prospective, randomized, multicenter trial. 2008 AANS/CNS Spine Section annual meeting, 2/08.
-
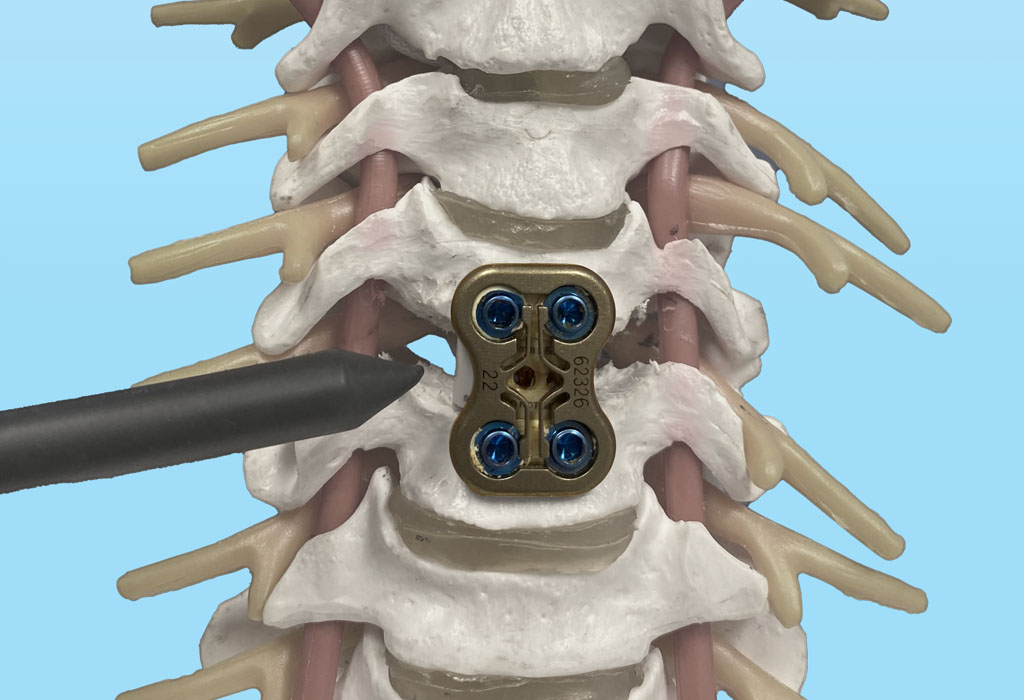
ANTERIOR CERVICAL DISCECTOMY AND FUSION (ACDF)
Dr. Wright performs ACDF surgery to relieve pain, numbness and weakness in the neck, shoulder, and arms, and to provide stability in the cervical (neck) portion of the spine.
Dr. Wright generally recommends an ACDF to remove a damaged disc that is causing pain due to compressed nerves or when there is excessive motion between the vertebrae. This can be due to a fracture or congenital anomaly, but most patients develop damage from progressive, chronic degenerative disease. Often, this occurs because of osteoarthritis or a herniated disc.
Procedure
Dr. Wright performs the ACDF procedure using a minimally invasive technique where he makes a small incision in the front (anterior) of the neck. This approach allows access the disc without disturbing the neck muscles and uninvolved spinal nerves.
The surgery itself is made up of two parts:
1. Discectomy – The damaged disc is removed through the small incision that was made. This eliminates pressure on the compressed nerve, thus relieving the pain and other symptoms the compression causes.
2. Fusion – A bone graft or implant device is inserted in the empty space where the damaged disc was to provide strength and stability to the area.
After the disc is removed, the space between the bony vertebrae is empty. To prevent the vertebrae from collapsing and rubbing together, a spacer bone graft is inserted to fill the open disc space. The graft serves as a bridge between the two vertebrae to create a spinal fusion. The bone graft and vertebrae are fixed in place with metal plates and screws. Following surgery, the body begins its natural healing process and new bone cells grow around the graft. After three – six months, the bone graft should join the two vertebrae and form one solid piece of bone. The instrumentation and fusion work together, similar to reinforced concrete.
Recovery
After fusion you may notice some range of motion loss, but this varies according to neck mobility before surgery and the number of levels fused. If only one level is fused, you may have similar or even better range of motion than before surgery. If more than two levels are fused, you may notice limits in turning your head and looking up and down. Motion-preserving artificial disc replacements have emerged as an alternative to fusion and Dr. Wright uses this technique whenever possible.

CERVICAL LAMINECTOMY
With a cervical laminectomy, your spinal canal in the neck area is enlarged through the removal of the lamina – the back part of a vertebra covering your spinal canal.
Dr. Wright performs a cervical laminectomy to relieve pressure on the spinal cord or nerves caused by bone spurs within the spinal canal. These bone spurs can narrow the space around your spinal cord and nerves, causing pain, weakness, or numbness that can radiate down your shoulders, arms, and hands.
While many patients can be successfully treated through one or more conservative methods, such as rest, nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, or the support of a neck brace, in some instances these treatments are insufficient. If the symptoms become progressively worse, Dr. Wright may recommend a cervical laminectomy.
Procedure
During a cervical laminectomy, Dr. Wright makes a small incision in your back directly over the affected area.
Depending on the extent of the damage, the lamina may be removed in portions or in its entirety on both sides of the spine. Typically, Dr. Wright will try to minimize the amount of excision to provide a minimally invasive intervention. However, sometimes the entire lamina is removed, depending on the extent of the damage. By removing the lamina, bone spurs, and other debris, the compression of the spinal cord and spinal nerves is alleviated, and symptoms improve.
The laminectomy procedure typically lasts one or two hours, depending on the extent of the operations and the number of involved levels of the spine.
Depending on your condition, Dr. Wright may also need to perform a spinal fusion of two or more vertebrae to better stabilize the spine, or a foraminotomy to widen the area where the nerve roots go through the spine.
Recovery
A laminectomy usually relieves much, or all of the pain and numbness patients suffer as a result of stenosis or disc herniation. The surgery is typically performed as either a same-day surgery or a one-night stay in the hospital. Soon afterward, a physical therapy regimen is initiated to build up muscle strength and flexibility. For several weeks following the procedure, activities will be restricted.

POSTERIOR CERVICAL FUSION
Posterior cervical fusion is the general term used to describe the procedure of mending two or more cervical vertebrae through an incision in the back (posterior) of the neck.
The procedure is a common one for patients who have cervical spine fractures or instability. Dr. Wright may also recommend a posterior cervical fusion to straighten the cervical spine and stop the progression of a spinal deformity, or to remove a tumor.
The goal of the procedure is to relieve pressure on the spinal cord and nerves, and to provide neck stability by fusing two or more vertebrae into one solid bone.
Procedure
During a posterior cervical fusion, Dr. Wright makes an incision in the back of the neck and places a bone graft along the sides of the injured section of the cervical spine. Over time, this bone graft fuses together to provide healing and greater stability. Metal screws and rods are sometimes used in conjunction with the procedure to extend fusion and/or provide immediate stability, as well as increase the likelihood of successful fusion.
Recovery
Recovery from a posterior cervical laminectomy and fusion surgery takes 8-12 weeks for the bones to heal, but patients continue to heal for up to a year after surgery. Walking is highly encouraged, immediately after surgery and throughout your post operative period. Most patients can return to a light desk job or household activities by 2-3 weeks after surgery. Patients with jobs that require heavy lifting, strenuous labor, or activities such as biking, skiing, or running will not be allowed to return until Dr. Wright ensures your bones have fused. This is usually around 12 weeks.

POSTERIOR C1-2 FUSION
Developed by Dr. Wright to reduce patient risk of injury.
The Posterior C1-2 Fusion procedure is one of the most common methods worldwide for treating disorders of the atlanto-axial complex and was actually developed by Dr. Wright during his tenure at Washington University in 2003.
The atlanto-axial complex refers to the top two bones of the neck (C1, the atlas, and C2, the axis) as well as the associated collection of ligaments that connect the bones together, and the blood vessels that travel through them to the brain.
This highly complex structure of bones and ligaments is where most of the rotation of the head occurs, and when damage occurs in this area – whether from trauma, tumor, inflammatory disorders, or congenital malformation – surgical repair is usually necessary.
Prior surgical techniques involved placing screws next to the vertebral arteries, which carried a risk of injury to the arteries carrying blood to the brain, and a small risk of stroke or death. Dr. Wright developed the technique to eliminate the risk by placing laminar screws in the posterior section (back of the neck) of C2, far away from the artery.
Procedure
Dr. Wright performs the surgery from the back of the neck, at the upper aspect of the spine. It is considered its own surgery (compared to a posterior cervical fusion) due to the unique anatomy and technical challenges there, mainly due to the position of the vertebral arteries.
Recovery
Posterior C1-C2 is performed on an in-patient basis. Most patients will spend two – three days in the hospital so they can be monitored for muscle spasms or incisional pain. After discharge, patients will also be required to wear a cervical collar for four weeks.